Tissue Engineering Research Group
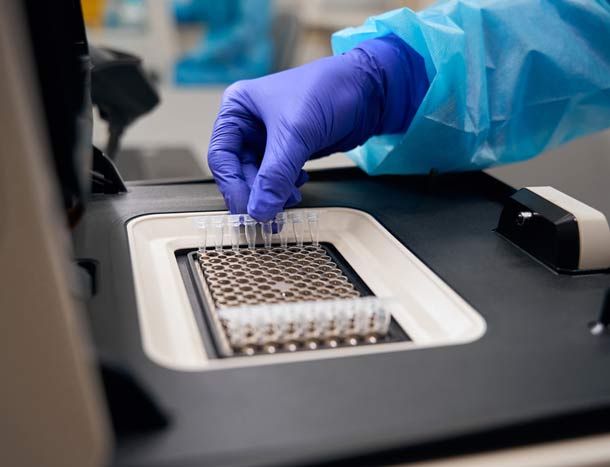
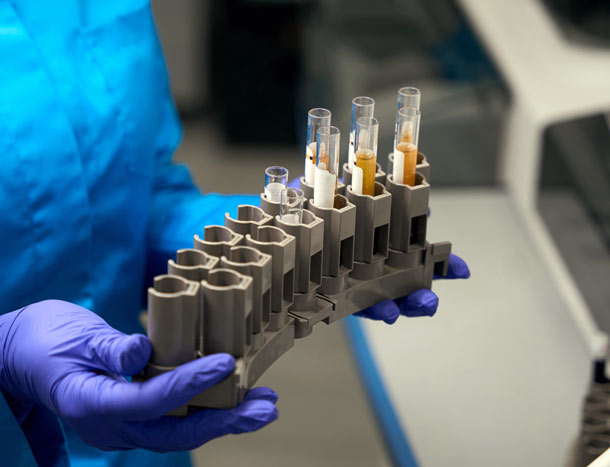
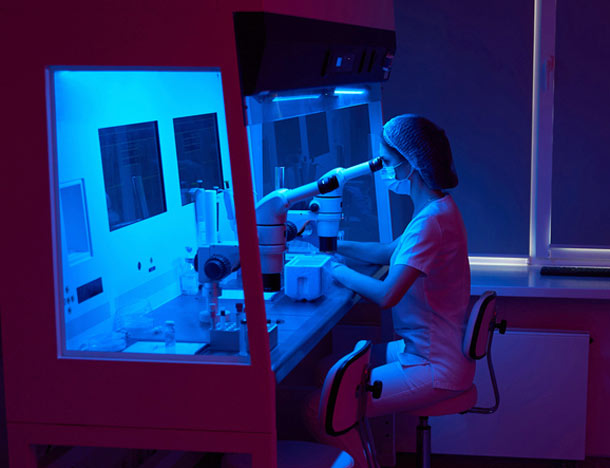
RCSI's Tissue Engineering Research Group (TERG) is a multidisciplinary research group focused on the development of cell and advanced biomaterial-based strategies for the repair and regeneration of bone, cartilage, skin, cardiovascular, ocular, respiratory, neural and other tissues.
Our researchers are also involved in medical device development and cutting-edge disease modelling. As part of the Department of Anatomy and Regenerative Medicine, TERG is closely linked with the School of Pharmacy and Biomolecular Sciences among others in RCSI.
Athena SWAN Bronze Award
We are proud to hold the internationally recognised departmental Athena SWAN Bronze Renewal Award for gender equality in higher education.
This award recognises RCSI's commitment to advancing gender equality and representation in the Department of Anatomy and Regenerative Medicine and TERG, and demonstrates the energy, commitment and collaborative culture that exists within these teams.
Learn moreInterested in collaborating or learning more about opportunities to work with TERG? Get in touch today to find out more.
Contact us Contact usWhat our researchers say

"I was very lucky to be in RCSI when TERG was first established. It has been amazing to see the growth and expansion of the group during that time ... The research is top-quality and it's a fantastic place to work."
Contact us
- Tel: +353 (0) 1 402 2100
- Email: TERG@rcsi.ie
- Address: Tissue Engineering Research Group, 123 St Stephen's Green, Dublin 2, Ireland
- Social media: Follow us on LinkedIn