What will you study?
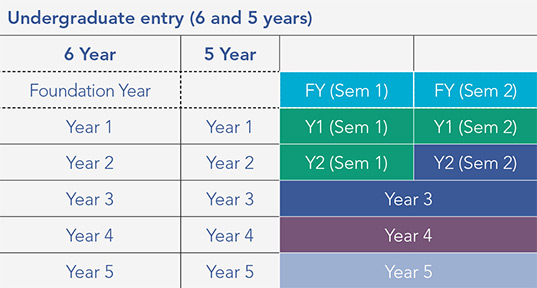
RCSI Bahrain's medicine programme has a five-year and six-year entry point. The six-year entry point provides a one-year preparation stage in advance of entry to the core five-year programme.
The Medicine programme for School Leavers and Mature Entry students is outlined below:
- Foundation Year (two semesters)
- Year 1 (two semesters)
- Year 2 (two semesters)
- Year 3
- Year 4 (Senior Cycle 1)
- Year 5 (Senior Cycle 2)
RCSI’s Medicine curriculum is innovative, future-focused and integrated. Our programme is centred around our students and is delivered in our state-of-the-art healthcare education facilities in Bahrain.
During your time with us you will be taught by RCSI academics, clinicians and researchers primarily in small groups or in an interactive manner when you are in large group settings. Your whole academic journey will be enabled and tracked by a dedicated e-portfolio system.
The Medicine programme is structured so that the focus is on knowledge and excellent clinical skills development. From day one, we also put intensive focus on the acquisition of clinical and communications skills, as well as understanding the central tenets of Personal and Professional Identity formation: professionalism, resilience and leadership. This ensures that you will be prepared for a personally and professionally demanding career in tomorrow’s healthcare environment.
RCSI’s Undergraduate Medicine programme is five years in duration. Depending on the qualifications presented at application, some students are required to complete an additional Foundation Year (six-year programme). Students may also enter through the Medical Commencement Programme (seven-year programme).
The five-year programme is structured as follows: Foundation of Practice (Y1 and Y2); Integration into Practice (Y3), and Preparation for Practice (Y4 and Y5). The programme has three vertical pillars of learning: Knowledge (Head); Skills (Hands), and; Personal and Professional Identity (Heart).
