Your journey
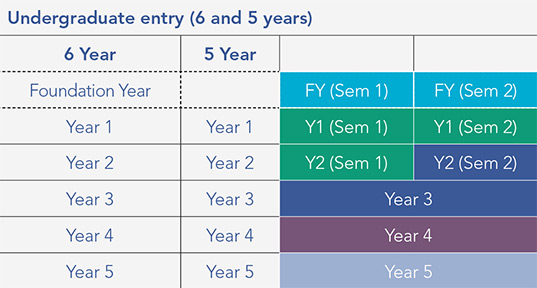
The Medicine programme for School Leavers and Mature Entry students is outlined below:
- Foundation Year (two semesters)
- Year 1 (two semesters)
- Year 2 (two semesters)
- Year 3
- Year 4 (Senior Cycle 1)
- Year 5 (Senior Cycle 2)
MB, BCh, BAO (Hons)
School of Medicine
The Medicine programme for School Leavers and Mature Entry students is outlined below:
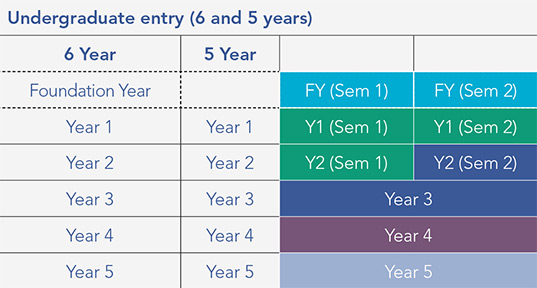
The five-year programme is organised into three stages:
The six-year track includes an extra Foundation Year before Year 1. Learning is built around three core pillars: Knowledge (Head), Skills (Hands), and Personal and Professional Identity (Heart). Below is a detailed outline of the modules you’ll study throughout the programme.
Case-based learning (CBL) is a core teaching and learning approach in Year 1 and 2. You will work in small groups and have the opportunity to choose from a wide range of tailored and credit-bearing student choice topics. These will allow for experiences that facilitate your personal growth.
Each medical student is assigned a personal tutor who supports them throughout their time at RCSI. The personal tutor programme aims to give students a safe space to reflect on their academic, personal, and professional progress; ensure they have access to the right supports and resources; guide them toward improvement; and encourage ongoing reflection, goal-setting, and lifelong learning. RCSI Medicine students are also placed in one of six learning communities, which comprise groups of students who are actively engaged in learning with and from each other. These communities have a cohort of students from every year in your programme and are an integral part of our teaching philosophy in the education of future healthcare professionals. The learning communities will allow you to build an academic relationship with your peers and to support each other in your learning. You will also be part of a broader inter-professional learning community made up of students from other programmes which facilitates participation in specific inter-professional academic activities.
At RCSI, our curriculum is informed by principles of positive education. This combines the science of positive psychology with curriculum development, delivery and assessment. As part of the core curriculum, students are taught skills and behaviours that encourage them to prioritise their health and well-being thus supporting their capacity to flourish. This approach to learning actively promotes positive growth, resilience and well-being.
Foundation Year (FY) consists of two semesters – delivered from September to May of the first year in the six-year Medicine programme.
FY will provide you with a solid grounding in the biomedical sciences and professionalism, as well as the necessary IT skills to operate efficiently within the University's virtual learning environment (VLE).
The course is delivered as a series of stand-alone modules taught in a single semester and integrated, systems-based modules, delivered across two semesters.
The FY structure is as follows:
First semester
Second semester
Both semesters
In Year 1, you will learn the basic anatomical, molecular and biochemical bases of human life, the principles of pharmacology, and acquire a basic understanding of the epidemiology and mechanisms of disease. You will also learn about musculoskeletal and skin systems, and how to diagnose and manage common and important cardiovascular and respiratory disease.
Student Choice modules will facilitate your exposure to various social and environmental experiences that will enable personal growth and the formation of your professional identity.
Case based learning (CBL) is a teaching tool used throughout Year 1. This is a learner-centered approach that involves interaction between students (up to 12). It focuses on the building of knowledge through group work.
CBL encourages the application of basic science knowledge, the linkage of knowledge between the basic and clinical sciences, a deeper understanding of content, and the development of clinical reasoning skills.
First semester
Second semester
Through an integrated teaching and learning approach, Year 2 modules are focused on ensuring that you gain the necessary knowledge and skills to communicate effectively and to work professionally and collaboratively to diagnose and manage common and important gastrointestinal and hepatological, central nervous system, endocrine and breast, renal and male and female genito-urinary diseases.
You will use an evidence-based approach that is grounded in best practice and safe patient care. Student Choice will continue to be integrated and you will have continuing opportunities to explore areas of interest such as innovation in research, education, global health, health systems and translational medicine. The Preparation for Clinical Placement module will teach you how to navigate the hospital environment prior to clinical placements in Year 3.
First semester
Second semester
During this year, your class will be divided and you will undertake prescribed modules at different times throughout the year. You will participate in hospital-based clinical placements and be located in one of the RCSI-affiliated teaching hospitals throughout Ireland. You will build on the knowledge and understanding of normal biology and diseases acquired during Years 1 and 2 and have the opportunity to apply this knowledge to real patients in multidisciplinary clinical settings.
Building on other relevant learning from Years 1 and 2, the New Horizons and Simulation module will provide you with the framework to interact and engage with a variety of new technologies that are being translated from the research to the clinical domain, including genomics and novel imaging approaches. You will also participate in a student selected component, where you complete an individual research or audit project.
Students will also have options relating to research projects overseas.
Year 3 modules
Year 4 modules will provide you with wide-ranging clinical exposure running in parallel with an integrated teaching and learning programme that focusses on knowledge and skills in areas including clinical competence, professionalism, communication, scholarship, leadership and global outlook.
You will be anchored full-time within a clinical team at an RCSI Teaching Hospital working in medicine, obstetrics and gynaecology, psychiatry, surgery, paediatrics, child health and general practice.
You will have the opportunity to practice your clinical skills and take an active part in the care pathways of individual patients, while simultaneously gaining experience in multi-disciplinary frameworks in both hospitals and community settings.
Year 4 modules
Year 5 will represent your final stage of preparation towards become a working clinician. Gaining clinical exposure and experience in the setting of a teaching hospital is a fundamental step towards ensuring competency in this professional role.
The clinical attachment block in Year 5 is the final mandatory clinical placement at an RCSI Teaching Hospital.
Clinical clerkship modules can be completed in any clinical discipline, although at least one of the two clerkship blocks must be completed in an acute hospital in the form of a sub-internship. There are also student elective options available outside Ireland.
The Preparation for Practice module (sub-internship) will allow you to demonstrate your ability to communicate effectively and professionally, as well developing your skills to manage challenging clinical scenarios and critical incidents through the application of leadership, professionalism, and resilience.
First and second semester
Meet Dr Gozie Offiah, Senior Lecturer and Director of Curriculum Implementation who explains our learning philosophy and how we integrate clinical and communication skills with knowledge acquisition and the formation of professional identity.
Your learning community will allow you to connect with students from other years, both academically and socially, throughout your programme. Learn more about the six communities in the School of Medicine and how they will shape your RCSI experience.
Find out about the wide range of teaching methods you will experience as an RCSI Medicine student. From our Anatomy Room, built more than 200 years ago, to our high-tech simulation labs – best practice and innovation are central to your learning.
Formative assessment will help you to track your progress and decide how best to integrate feedback during your learning journey. Engagement with your personal tutor and your personalised e-portfolio will support your progress.
Learn more about our wide range of student supports available to you. We have a large multidisciplinary team that can help you to overcome educational challenges and provide training and guidance as well as practical and emotional support.
Discover how your exposure to clinical experiences at the earliest stages of your programme will shape your learning at RCSI. You will take increasing levels of clinical responsibility throughout your degree and experience domiciliary, community and hospital care settings.
RCSI places a high value on supporting international clinical experiences for our students. Accordingly – through a network of international partnerships with other world-leading universities and healthcare institutions – we offer a significant number of clinical elective opportunities.
Learn more about the RCSI Research Summer School, research electives and other intensive experiences that allow you to be exposed to core research skills in topics such as scientific writing, presentation, data management, statistics and ethics.